Can Infectious Disease Be Cured?
Humans and microbes have always coexisted. In fact, we often benefit from each other. Microbes live happily in our bodies, helping us perform vital functions and protecting us from harmful intruders. However, sometimes microbes hurt us in the form of infections that damage our bodies and spread from person to person.
When the relationship between humans and microbes sours, infectious disease ensues.
But can infectious disease be cured?
That question has a simple answer with a lengthy explanation: no, it technically cannot be cured, but it can be prevented, treated, and even eradicated through vaccines, research, and community mobilization.
Read on to learn what an infectious disease is, how it spreads, and what researchers and doctors are doing to treat, prevent, and eradicate each one.
What is an Infectious Disease?
So when does our interaction with microbes turn into an infectious disease? And does all infection imply illness?
To understand what exactly an infectious disease is and the different types of infectious diseases, let’s break down a few key terms:
- Microbes are highly adaptable microorganisms that have colonized this world and our bodies, greatly outnumbering the human cells in our gut, and often aiding in essential functions like breaking down food, synthesizing vitamins, and stimulating the immune system. Most of these are harmless—those that aren’t are called pathogens.
- A pathogen is the microbe that causes a disease. The pathogen’s virulence is the severity of the disease’s symptoms.
- An infection is when pathogens, or pathogenic microbes, invade and multiply in the body—however, infection doesn’t inherently result in disease.
- A disease only occurs when infections harm the body’s essential systems or functions.
Therefore, an infectious disease is simply one where harmful pathogens damage an individual’s vital bodily functions or systems—and one that is communicable. A communicable disease is one that can be passed on from person to person, versus a non-communicable disease, which is chronic and non transferable, like cancer or heart disease.
Types of Microbes
Infections occur when microbes enter an individual’s body and start multiplying. However, not all microbes are created equal.
In fact, there are four main types that cause an infection:
- Bacteria – Ancient beings, bacteria are incredibly adaptable, highly varied, and at times, exceedingly harmful. Bacterial infections can cause urinary tract infections, tuberculosis, and strep throat.
- Viruses – These are 10 to 100 times smaller than bacteria and often far trickier to treat. A viral infection is different from a bacterial infection. They are no more than tiny protein-protected packets of either RNA or DNA, and can only reproduce when attached to a living host cell. Viruses are behind the likes of chickenpox, measles, HIV, SARS, and more.
- Fungi – These fun guys (pun intended) are spore-forming microbes that vary from ringworm to mold.
- Protozoa, prions, and helminths – These are the parasitic worms, agents, and proteins responsible for the likes of dysentery, malaria, hookworm, and more.
How Pathogens Enter the Body
The damage of infectious diseases depends on how they enter the body and, therefore, how they spread throughout a population.
There are four primary sites through which pathogenic microbes can enter their human host:
- Skin – Open cuts or breaks in the skin can let in nasty pathogens, like the ones which cause tetanus, for example.
- Urogenital Tract – Common way for sexually transmitted diseases to enter the body.
- Gastrointestinal – Pathogens can also enter through the mouth oral cavity.
- Respiratory Tract – The influenza virus, for example, enters through the mouth and nose.
Knowing how a contagious disease is transmitted helps scientists and disease control organizers target, track, and control an infection.
How Pathogens Spread
To wrangle and eradicate infectious disease, researchers have to uncover how pathogens spread within a population using four main categories:
- Vectors – This term describes any creature that transmits disease, like the dreaded mosquitoes that spread yellow fever and malaria. Other vectors can be ticks, fleas, dogs, snails, and mites.
- Contact – Some pathogens are transmitted through direct—or indirect—contact with infected mucous membranes, bodily fluids, and skin. Indirect contact may include touching a countertop, doorknob, or other surface that an infected person previously touched, followed by contact with the eyes, nose, or mouth.
- Common Vehicles – These can be contaminated water sources, blood, food, or any physical fluid or object that can spread pathogenic microbes. For example, Salmonella enters the digestive system through contaminated food and water.
- Air – Sci-fi movies love to depict this type of spread—airborne diseases are particularly frightening because they spread from dust particles, droplets, or residue that floats in the air for a long time. The rubeola virus, which causes measles, is one example of an airborne pathogen.
How Infectious Diseases Make People Sick
The spread of an infection from person to person does not inherently mean they will get sick. Here’s how an infection becomes harmful:
- The infection reaches a vulnerable site in the body and damages cells.
- The pathogen triggers a response from the body’s immune system.
- The immune system combats the infection, causing additional symptoms like headache, fatigue, fever, or rashes.
- In some cases, the immune response is excessive, resulting in “friendly-fire.” The immune system attacks both infected and uninfected cells, simultaneously damaging otherwise healthy tissue.
An immune response can vary from person to person. If the infection survives the immune system’s defenses, it will continue to spread and harm the host. If the infection survives the immune system’s defenses, it will continue to spread and harm the host.
In sum, the symptoms of “feeling sick” in an infected person are a result of both the cell damage caused by pathogens and the immune system’s response.
Types of Outbreaks
When an infectious disease begins to affect multiple people in a population, disease control specialists and public servants have to label this spread using various epidemiological terms, including:
- Outbreak – An outbreak indicates a rapid (or faster than anticipated) spread of infectious disease cases (of the same type and strain) in a given area. If not handled quickly, outbreaks can swiftly turn into a dangerous epidemic.
- Endemic – This term describes the constant presence of a disease, ailment, or issue in a specific country, population, or geographic location.
- Epidemic – Epidemics describe an infectious disease that has spread widely across a population, region, or community within a country.
- Pandemic – A pandemic is an epidemic, multiplied. Pandemics occur when an epidemic affects multiple countries or even continents. (i.e. the covid 19 pandemic)
How to Combat Infectious Diseases
With an arsenal of information on our side—and newfound details on how certain diseases spread, enter the body, and harm individuals—vigilant researchers have everything they need to treat infectious diseases and attempt to eradicate them entirely.
So, how do scientists tackle these stubborn travelers?
The answer: a lot of research and even more hard work. Scientists can use flow cytometry in studying infectious disease, which we will explore later in this article.
There are a few important ways that specialists deal with infectious diseases:
- Vaccines – Vaccines introduce dead or weak forms of a pathogenic microbe into the body, which kick starts the immune system and trains it to identify, eliminate, and “remember” the pathogen later. Vaccines are responsible for the near-eradication of once-common ailments like measles, polio, and whooping cough in the U.S.
- Antibiotics – These medicines combat a bacterial infection by either destroying it or halting its reproduction. Unfortunately, bacteria are highly adaptable and can evolve strains that are antibiotic-resistant.
- Antivirals – Antiviral drugs target viruses, which are trickier than bacteria because they are self-sufficient and unable to be artificially cultured for research purposes. While antibiotics can treat a wide swath of pathogens, antivirals have to be targeted to specific viruses.
- Awareness – Education, announcements, and awareness on proper hygienic practices, immunization, and food handling are keystones of disease prevention. The public has to become increasingly aware of how to properly handle animals, conduct safe sex practices, and respond to disease threats.
- Food Safety – By properly handling food through vigilant manufacturing, packaging, and agricultural practices, foodborne diseases can be almost entirely prevented from affecting the public.
- Disease Control – Government entities, like the U.S. Center for Disease Control (CDC), actively respond to outbreaks and work on preventative measures like vaccinations, surveillance, and tracking to improve public health and stop the spread of infectious disease.
The fight against infectious disease depends on the development of emerging technologies that help study these pathogens more effectively. Understanding how to study infectious disease through various methods is a great place to start.
Using Flow Cytometry to Get the Upper Hand on Infectious Disease
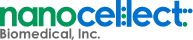
One necessary process in infectious disease research is cell sorting, which is aided by a key piece of technology: the flow cytometer.
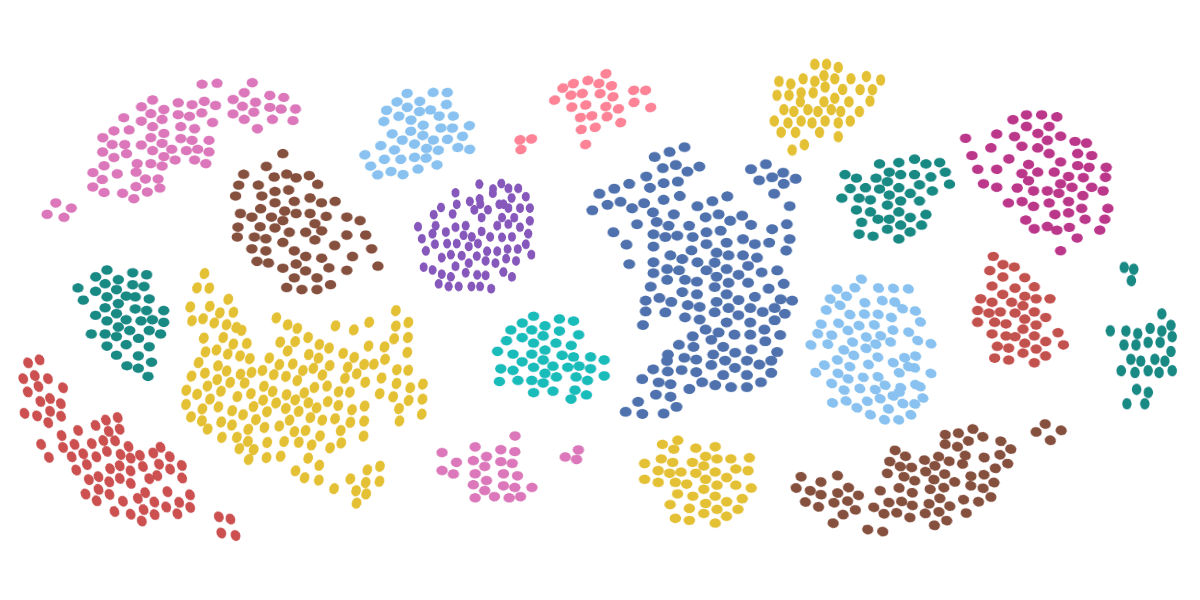
Flow cytometers sort and isolate infected cells using a combination of hydrodynamic properties, laser optics, and electronic systems. Cell populations are combined with fluorescent biomarkers and then identified one at a time, in rapid succession. To achieve this enormous (or, in this case, microscopic) feat, flow cytometers have to be incredibly precise, quick, and most importantly, gentle with cell samples.
With traditional flow cytometers, the pressure needed to accomplish the cell sorting was enough to rupture the cell wall and cause cell death. Yet, every sample is precious, and to produce clear data, researchers need to preserve as much of the sample as possible.
That’s where NanoCellect comes in.
For a Happy, Healthy Culture, You Need Happy, Healthy Cells
NanoCellect’s state-of-the-art WOLF G2 Cell Sorter and N1 Single-Cell Dispenser allow in-lab teams to make unprecedented progress when studying infected cells, through uniquely gentle and intuitive sorting methods.
NanoCellect rises above other traditional cell sorters because:
- They are safe, sterile, and intuitive, so researchers at all levels can handle infected cells with care.
- They isolate cells at a pressure of less than 2 psi—this is 30 times gentler than traditional flow cytometers, dramatically increasing viable cell populations.
- The disposable cartridges used for cell sorting prevents sample-to-sample contamination.
For research equipment built to treat cells gently, think NanoCellect.
Sources:
ACPHD. Communicable Disease. http://www.acphd.org/communicable-disease.aspx
NCBI. What You Need to Know About Infectious Disease. https://www.ncbi.nlm.nih.gov/books/NBK209710/
NCBI. Prevention and Treatment. https://www.ncbi.nlm.nih.gov/books/NBK209704/
NCBI. Q&A: What are pathogens, and what have they done to and for us? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5648414/
Microbiology Society. Microbes and Disease. https://microbiologysociety.org/why-microbiology-matters/what-is-microbiology/microbes-and-the-human-body/microbes-and-disease.html