How Do We Study Infectious Disease?

Before the emergence of penicillin in 1941, “household” diseases that we are now cavalier about were life threatening. Less than one hundred years ago, strep throat, that common throat irritant many children experience and subsequently spread (like wildfire) through their school, was fatal when left untreated.
Ear infections, whooping cough, and pneumonia had similar fates. Up to 90% of children with bacterial meningitis died without access to life-saving antibiotics!
Thankfully, today there are dozens of different antibiotics that doctors can choose from to treat these illnesses. But this doesn’t mean scientists have solved the mystery of infectious diseases.
On the contrary, there are still great bounds of discovery awaiting in the study of disease.
Branches of Study Involved in Disease
To understand and dissect the complex nature of disease, all levels of analysis must be considered. Moving upwards in scope, understanding a disease involves:
- The nanoscopic level – Decoding the DNA of bacteria, viruses, fungi
- The microscopic level – Understanding the cell structure and its components to determine how it functions
- The individual level – How infectious diseases spread throughout an individual’s body and how the immune system reacts
- The population level – How infectious diseases spread from individual to individual throughout a population
Each of these levels of analysis play a role in understanding infectious diseases.
For example, if you wanted to know how dangerous a particular pathogen was, you might analyze the infectious disease at the individual level. While if you wanted to create a drug that disrupted the pathogen’s ability to reproduce, you might look at the microscopic or nanoscopic level. But if you wanted to understand whether a disease warranted nation-wide concern (or in the case of COVID-19, global concern), you need to rely on population studies, infection vectors, and transmission rates.
These different forms of studying infectious diseases are consolidated in different branches of study. Moving in the reverse direction of scope:
- Large-scale population studies of infectious diseases, how they’re transmitted, and at what rate they’re transmitted are done with epidemiological studies.
- An individual immune response and how particularly harmful a pathogen is depends on immunology—an intersecting branch between the medical and biological sciences.
- Studying bacterial infection (strep throat, ear infections, meningitis, etc.) and their respective pathogens are studied through the lens of bacteriology.
- Viruses and their subsequent diseases are considered a much more difficult code to crack when compared with bacterial diseases. These are studied in the field of virology.
Because of the differences in scale, each branch comes with a unique methodology.
Epidemiology: Populational Studies of Infectious Disease
When studying large populations of people, there are three methods of epidemiological studies:
- Descriptive studies
- Analytic studies
- Experimental studies
These methods are not isolated; in fact, they’re often used chronologically. Descriptive studies are used to create a description of an unknown disease. Analytic studies take that description, isolate the disease, and further study it. Once enough information is available, experimental studies develop and test hypotheses about the disease in question.
Let’s explore each of these in detail.
Descriptive Studies
Descriptive studies focus on three important questions of a disease: When, Where, and Who.
When: Time Trends of a Disease
There are four time trends that can be used to understand a disease.
- Secular trend: These time trends are over large periods of time (years). For example, when looking at the smallpox outbreak, while there are spikes and dips throughout the last hundred years, overall the secular trend shows a decline toward eradication.
- Periodic trend: These trends are used for recurring ailments. The flu is a periodic virus that even has a known “flu season.”
- Seasonal trend: Some diseases are more prevalent in certain seasons. Food-borne illnesses are more commonly found in the summer when high heats cause food to spoil and bacteria to grow more easily.
- Epidemic occurrence: This time stamp is used when a shift in factors that support transmission arise and cause an epidemic outbreak of an infectious disease.
Where: The Location of a Disease
The location of a disease takes into account three different locations:
- Where the host was when they showed symptoms of the disease.
- Where the host was when they became infected
- Where the source of the disease was infected
Who: The Demographic of the Infected
The third important question of a descriptive study depends on who was infected. What characteristics set them apart from other possible factors, including:
- Age
- Sex
- Economic status
- Compromising immune system factors
- Employment
- More
Combining the When, Where, and Who offers a substantial amount of data to then be analyzed.
Analytic Studies
When conducting analytic studies of populations, there are two main methods: case-comparison and cohort.
- Case-Comparison Method – Also known as case-control method, this analytic study involves comparing the group of infected individuals with those of similar demographics who are not infected.
- Cohort Method – The cohort method involves how groups of infected and non-infected individuals were in contact with other infected individuals. This isolates the methods of transfer.
The point of analytic studies is to take the large amounts of data coming from descriptive studies and start to isolate certain characteristics of a disease. From there, researchers can start to build informative arguments about what a disease is.
Experimental Studies
Experimental studies build and test hypotheses about the disease.
For example, when a drug treatment is designed to match the characteristics of an infectious disease, this must be tested rigorously in animal and human trials. Once the results are in from the drug trials, the efficacy of the drug will be determined, and it will either confirm or reject the hypothesis.
Microbiology: The Study of Individual Pathogens
While epidemiological studies range from global population studies down to the individual (immunological) studies, there’s another way to approach infectious diseases—researching the individual pathogens.
The study of infectious diseases from a microbiology standpoint involves decoding the physical characteristics of the microbe. Further studies then decipher:
- The structural model of the emerging pathogens
- How the pathogen interacts with healthy cells
- Methods of treatment
The microbiological laboratory techniques used to gather this information involves:
- Lab prep: sterilization, disinfection, and sanitization
- Setting up the cultures
- Fixing and staining the cultures for identification
Lab Preparation
When studying infectious pathogens, there are a number of biosafety concerns to consider and prepare for. The CDC ranks these biosafety concerns based on the risk factors of the microbes being studied. There are four levels of safety measures from BSL-1 up to BSL-4 that determine the safety equipment needed, the protocols to put in place, and the security of the facility.
From there, the equipment used needs to be sterilized prior to use—this avoids cross-contamination.
Setting up the Cultures
Cultures are what allow microbes, bacteria and other infected cells, to grow into large enough populations to be studied effectively. This requires a basic procedure called the five I’s:
- Inoculation – The microbes are placed in a sterile medium with nutrients to allow growth
- Incubation – The microbes are then allotted time to grow
- Isolation – The microbes are then isolated and separated
- Inspection – Researchers then look for growth characteristics
- Identification – The species of the microbes are then identified under a microscope
Staining the Cultures
Not all microbes are large enough to be identified with a microscope. In the cases where the sample is too small, stains are used. Simple stains are basic dyes that make it easier to see the shape and structure of a cell. Differential stains use multiple dyes to help researchers better identify bacteria.
Infectious Viruses
Viruses are a different challenge from bacteria. This is because viruses aren’t living organisms—they’re packets of nucleic acids within a protein structure. As such, researchers have gotten creative in their methods of study.
Some of the most common ways to study viral diseases are through:
- Detection of immune response – Because viruses will often have similar physical symptoms, it’s hard to determine the virus based on retrospective studies. Indirect methods offer light into the antibody response, which can help isolate and identify the virus. Some of these methods include: virus neutralization, hemagglutination inhibition, and enzyme linked immunosorbent assay (ELISA).
- Light and electron microscopy – Viruses are a couple orders of magnitude smaller than bacteria—meaning the chances of viewing a virus under a microscope are, well, none. Unless of course you use a light or electron microscope. These technologies allow a visual representation of the viruses to be seen and analyzed.
- Infecting cell culture or fertile eggs – Researchers are able to isolate a virus and allow it to spread through cell cultures or fertile embryos. These isolation methods are less specific and often lead to novel discoveries.
Cell Research Made Easy
Studying infectious diseases can be grouped into two categories. Epidemiological and immunological studies measure population and individual response to diseases, while microbiological studies measure properties of the individual pathogen. Both are necessary to round out the knowledge of an infectious disease.
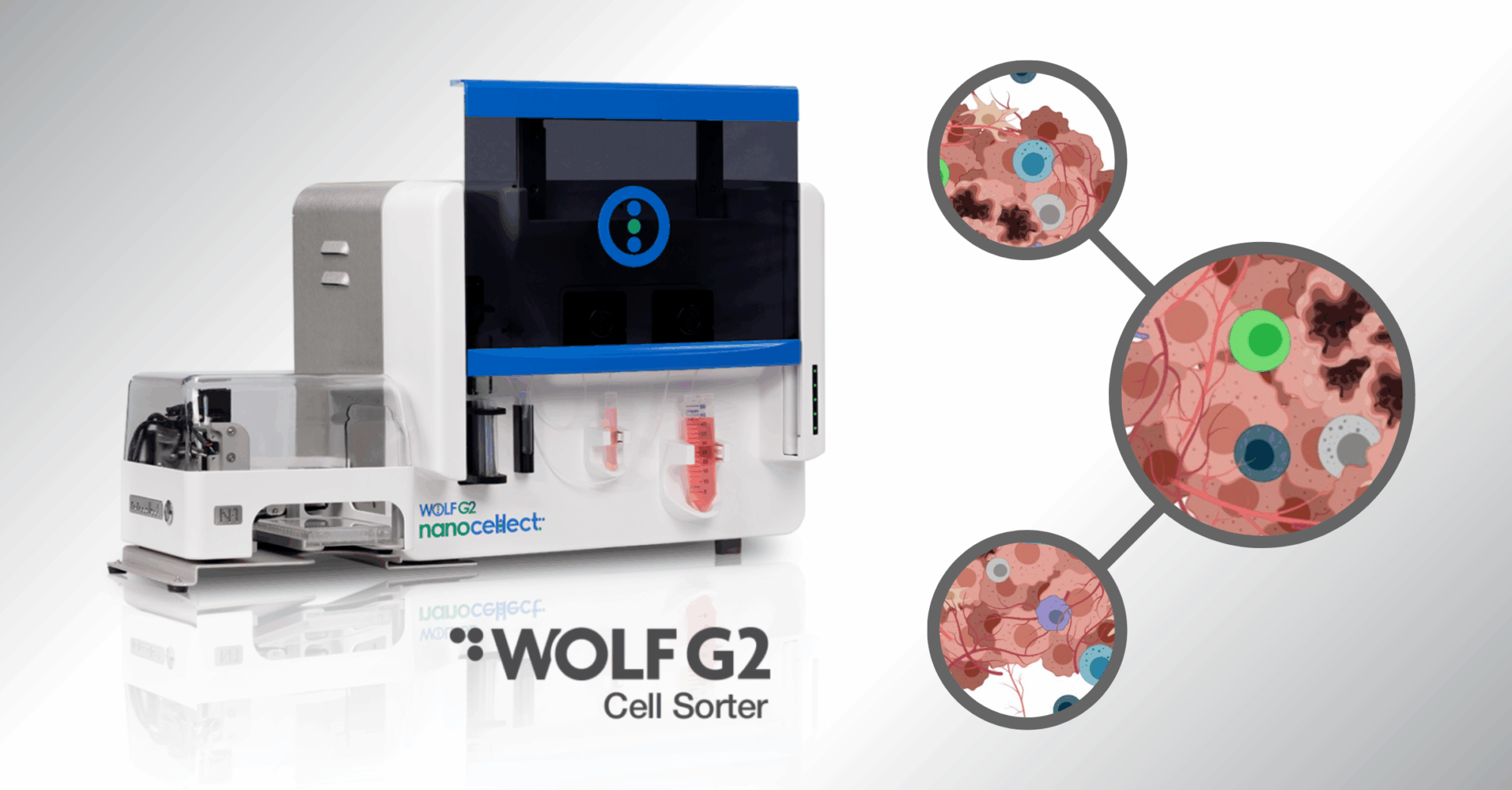
When studying at the microbe level, one of the most important aspects is the isolation phase. To ensure the samples are homogenous, researchers need a way to sort the infected cells or bacteria—without damaging the cells.
That’s where cutting-edge technologies, like the NanoCellect WOLF G2 Cell Sorter, enter the picture. Using sorting pressures of less than 2 psi (which is ten times gentler than the next leading flow cytometer), researchers have access to an efficient cell sorter that doesn’t compromise their research data.
Plus, with NanoCellect’s disposable cartridges, there’s zero chance of cross-contamination between sortings.
If you’re interested in how NanoCellect can improve your lab with efficient cell sorting, next generation sequencing such as single-cell genomics, cell line development, and antibody discovery, reach out to the experts today.
Sources:
- HealthyChildren.org The History of Antibiotics. https://www.healthychildren.org/English/health-issues/conditions/treatments/Pages/The-History-of-Antibiotics.aspx
- NCBI. Chapter 9 Epidemiology. https://www.ncbi.nlm.nih.gov/books/NBK7993/#:~:text=The%20three%20major%20epidemiologic%20techniques,used%20most%20is%20descriptive%20epidemiology
- Our World in Data. Smallpox: disease, transmission & symptoms. https://ourworldindata.org/smallpox#smallpox-disease-transmission-symptoms
- Clinical Gate. Microbiological Laboratory Techniques. https://clinicalgate.com/microbiological-laboratory-techniques/#s0140
- CDC. Recognizing the Biosafety Levels. https://www.cdc.gov/training/quicklearns/biosafety/
- MECC. The Methods for Studying Microorganisms. https://water.mecc.edu/courses/ENV295Micro/Lesson4_print.htm
- Agrilife. Virology Techniques. https://agrilife.org/vetmed/files/2012/10/LS_5_4_sample_lesson.pdf