A 2021 publication in Nature from the labs of Drs. Rathmell at Vanderbilt University investigated the metabolism of cancer cells and immune cells in the tumor microenvironment, specifically focusing on glucose and glutamine uptake. Here’s an overview of what the tumor microenvironment is and how the WOLF Cell Sorter was used for this customer’s research.
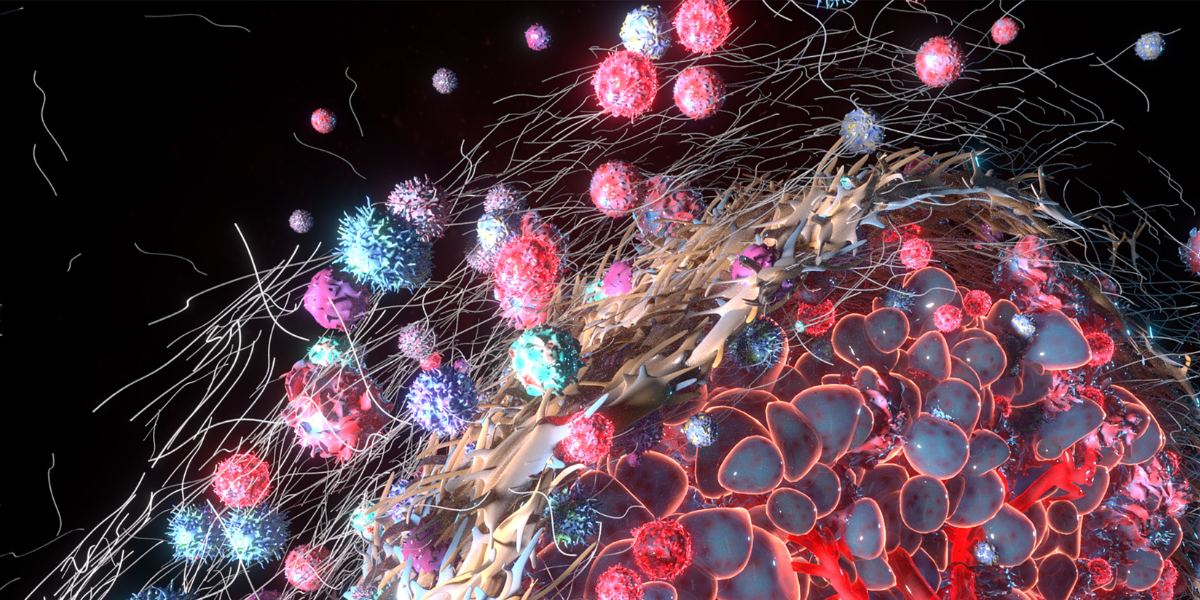
The tumor microenvironment (TME) refers to the surrounding environment in which a tumor exists, including the surrounding blood vessels, immune cells, fibroblasts, and extracellular matrix. The TME is a complex and dynamic system that interacts with cancer cells and plays a crucial role in tumor growth, invasion, and metastasis.
The TME can vary depending on the type and location of the tumor. Still, it generally includes immune cells that can promote or inhibit tumor growth, blood vessels that supply the tumor with nutrients and oxygen, and stromal cells such as fibroblasts that produce the extracellular matrix that provides structural support for the tumor.
The TME can also be influenced by factors such as inflammation, hypoxia, and acidosis, which can impact tumor growth and response to therapy. Understanding the TME is important for the development of new cancer treatments that target the interactions between cancer cells and their environment.
Positron emission tomography (PET) is a medical imaging technique that can be used to measure glucose metabolism in the body. The process involves using a radioactive tracer that is similar to glucose, such as 2-[18F]fluoro-2-deoxy-D-glucose (FDG), which is injected into the bloodstream.
Once in the body, the FDG is transported into cells through glucose transporters, which are proteins on the cell membrane that help glucose enter cells. Once inside the cells, the FDG is phosphorylated by an enzyme called hexokinase and trapped in the cell, where it undergoes further metabolic processes.
The radioactive tracer emits a positron, which is a positively charged particle that quickly interacts with an electron in the surrounding tissue. The interaction produces two gamma rays, which are detected by the PET scanner. By detecting the gamma rays, the PET scanner can determine the location and amount of the radioactive tracer, which reflects the amount of glucose that is being metabolized in the body.
Cancer cells have higher rates of glucose metabolism compared to normal cells, due to the Warburg effect. This makes FDG a useful tracer for detecting and monitoring cancer, as cancer cells will accumulate more FDG than normal cells. PET scans can provide information on the location and size of tumors, as well as the metabolic activity of cancer cells. This information can be used to diagnose cancer, monitor treatment response, and detect recurrence of cancer.
The Warburg effect refers to a metabolic phenomenon where cancer cells consume glucose at a much higher rate than normal cells and convert it into lactate, even in the presence of sufficient oxygen. This is in contrast to normal cells, which preferentially use oxygen to generate energy through oxidative phosphorylation.
It was first observed by Otto Warburg in the 1920s and is now known to be a hallmark of cancer metabolism. Cancer cells rely on glycolysis, the breakdown of glucose, to produce energy, even under aerobic conditions. This results in the accumulation of lactate and other byproducts, which can contribute to tumor growth and survival.
The Warburg effect is thought to be driven by various factors, including alterations in oncogenes and tumor suppressor genes, as well as changes in the TME, such as hypoxia and inflammation. The upregulation of certain enzymes and transporters involved in glycolysis, such as hexokinase and glucose transporters, also contributes to the Warburg effect.
This has important implications for cancer diagnosis and treatment, as it provides a potential target for developing new cancer therapies. By targeting the metabolic pathways that are upregulated in cancer cells, it may be possible to selectively kill cancer cells while sparing normal cells.
This brings us to the publication in Nature from the labs of Drs. Rathmell at Vanderbilt University. They investigated the metabolism of cancer cells and immune cells in the TME, specifically focusing on glucose and glutamine uptake. Using PET tracers, Reinfeld et al. found that a subset of immune cells called myeloid cells had the greatest capacity to take up glucose, followed by T cells and cancer cells, while cancer cells had the highest glutamine uptake.
The researchers injected mice with radioactive 2-NBDG and used the WOLF Cell Sorter to sort cells obtained from tumor tissue. 2-NBDG (2-(N-(7-nitrobenz-2-oxa-1,3-diazol-4-yl)amino)-2-deoxyglucose) is a fluorescent glucose analog that has been widely used to measure glucose uptake in cells and tissues. One of the unique features of the WOLF is that it uses sterile, single-use, disposable microfluidic cartridges for single cell dispensing and isolation. Since the entire fluidics line is contained within the cartridge setup, the WOLF is ideal for isolating cells from samples that contain radioactive compounds, which would not be compatible with cell sorters in a shared resource lab, for example.
The Vanderbilt team observed that when they inhibited glutamine uptake, there was increased glucose uptake across all cell types in the TME, indicating that glutamine metabolism suppresses glucose uptake. These findings suggest that cell-intrinsic programs drive the preferential acquisition of glucose and glutamine by immune and cancer cells, respectively, and highlight the potential for exploiting these metabolic differences to develop targeted therapies and imaging strategies for specific cell populations in the TME.
Understanding the TME is crucial for the development of new cancer treatments that target the interactions between cancer cells and their environment. By using the WOLF Cell Sorter, researchers at Vanderbilt University were able to sort radioactive samples for cancer and immune cells in order to study their glucose metabolism using downstream assays that required the cells to be intact and viable.
Do you have a challenging sample type that you’re not able to sort using a shared flow cytometer? Get in touch with us at [email protected]!





